Peripheral vascular disease (PVD) is a progressive disorder that restricts blood flow to the arms, legs, or other body parts. It occurs when blood vessels narrow, become blocked, or spasm. It can lead to pain and cramping.
PVD describes the reduced circulation of blood to a body part (not including the brain or heart). If PVD occurs only in the arteries, it is called peripheral artery disease (PAD). Most cases of PVD affect the arteries, so research often uses the terms interchangeably.
In this article, we look closely at PVD, including its causes, symptoms, diagnosis, and treatments.
Fast facts on PVD
- PVD affects
more than 20% of individuals who are 80 years old or older. - Common risk factors include being over the age of 50 years, having diabetes, smoking cigarettes, and having high blood pressure or high cholesterol.
- Common symptoms include pain and cramps in the legs, hips, and buttocks.
- According to the
Centers for Disease Control and Prevention (CDC) , PVD affects men and women equally. - Arteriosclerosis and atherosclerosis are among the most common causes of PVD.
Signs and symptoms of PVD often appear gradually. They occur more commonly in the legs than in the arms because the blood vessels in the legs are further from the heart.
Typical symptoms of PVD include feeling pain, aches, or cramps while walking. However, up to
These pains, aches, and cramps related to physical activity are referred to as claudication, and they can occur in the following areas:
- buttocks
- calf
- hip
- thigh
Symptoms of claudication often develop when someone is walking for longer distances or exercising. The symptoms typically go away with rest. However, as PVD progresses, symptoms may get worse and become more frequent. Leg pain and fatigue may persist even while resting.
Other symptoms of PVD can include:
- leg cramps when lying down
- hair loss on the legs
- skin that is cool to the touch
- thin, pale, or shiny skin on the legs and feet
- slow-healing wounds and ulcers
- cold, burning, or numb toes
- weak or absent pulse in the feet
- sensations of heaviness or numbness in the muscles
- atrophy, which is the wasting away of muscle (in severe cases)
Causes of PVD vary and depend on the type a person has.
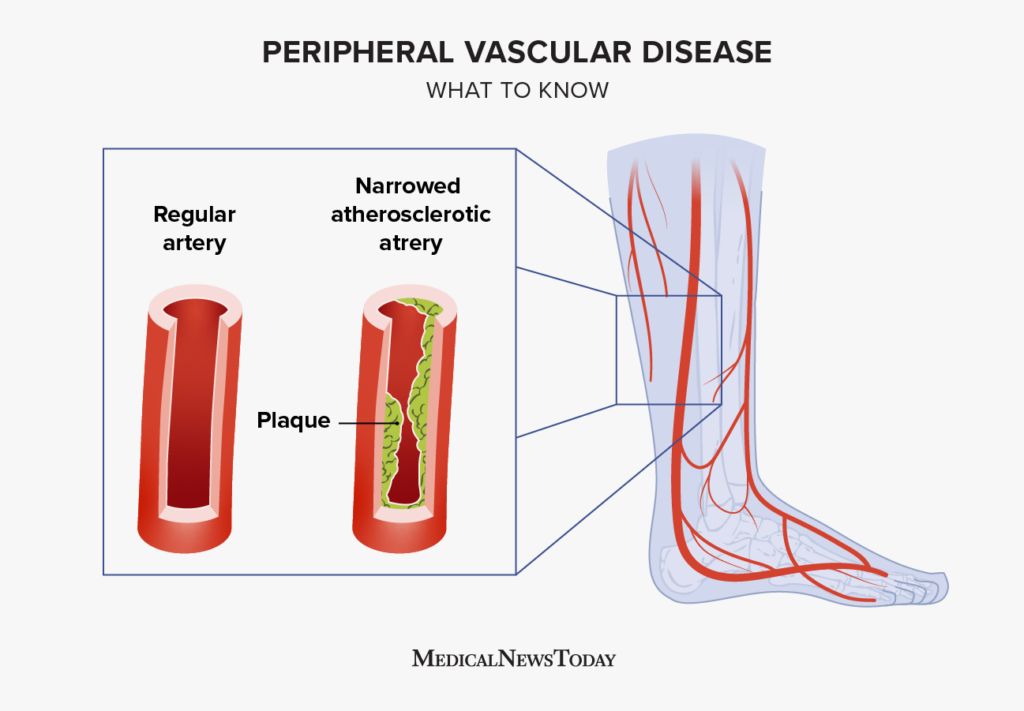
Arteriosclerosis, which is due to changes in the structure of the blood vessels, is the most common cause of PVD.
Atherosclerosis occurs when plaque (fats and other substances) builds up in the blood vessels. Atherosclerosis can restrict blood flow and, if left untreated, cause clots. Clots block the arteries and can cause loss of limbs or organ damage.
Common risk factors for atherosclerosis include:
- high blood pressure (hypertension)
- high cholesterol or triglycerides
- inflammation from arthritis, lupus, or other conditions
- insulin resistance
- smoking
The following conditions may also cause structural changes in the blood vessels:
- Buerger’s disease
- chronic venous insufficiency
- deep vein thrombosis (DVT)
- Raynaud’s disease
- thrombophlebitis
- varicose veins
Injury, inflammation, or infection in the blood vessels may also cause structural changes in the blood vessels.
In general, the risk factors for PVD are similar to those for arteriosclerosis. They
- Age: People ages 50 years and over are more likely to get PVD and PAD.
- Obesity: Living with obesity increases the risk of arteriosclerosis, PVD, and other cardiovascular conditions.
- Lifestyle choices: Smoking, substance use, a sedentary lifestyle, and following a diet lacking nutrients may increase a person’s risk of PVD.
- Medical and family history: PVD risk increases for people who have a history of cerebrovascular disease or stroke. Those with a family history of high cholesterol or hypertension are also at higher risk.
- Other medical conditions: People with high cholesterol, hypertension, heart disease, or diabetes are at an increased risk of developing PVD.
- Race and ethnicity: African Americans tend to develop PVD
more frequently .
If a person suspects they have PVD, it is essential that they see a doctor. Early diagnosis and treatment can improve the outlook for the disease and prevent severe complications.
A doctor will diagnose PVD by:
- taking a full medical and family history, which includes looking at lifestyle, diet, and medication use
- performing a physical examination, which includes checking the skin’s temperature and appearance and looking for a pulse in the legs and feet
They may also order tests to confirm a diagnosis or rule out other conditions. Several other disorders can mimic the symptoms of PVD and PAD.
Tests used to diagnose PVD include:
- Angiography: This test involves injecting dye into the arteries to identify a clogged or blocked artery.
- Ankle-brachial index (ABI): This noninvasive test measures blood pressure in the ankles. The doctor then compares this reading to blood pressure readings in the arms. A doctor will take measurements after rest and physical activity. Lower blood pressure in the legs suggests a blockage.
- Blood tests: Although blood tests alone cannot diagnose PVD, they can help a doctor check for conditions that can increase a person’s risk of developing PVD, such as diabetes and high cholesterol.
- Photoplethysmography (PPG): A PPG is a noninvasive test to monitor heart rate. A light source and a photodetector are placed on the surface of the skin to measure variations of blood circulation.
- Treadmill exercise test: During this test, a person walks on a treadmill while the speed is steadily increased. If a person indicates pain at a certain threshold, this may be a sign of PVD or PAD.
- Computed tomography angiography (CTA): A CTA test shows the doctor an image of the blood vessels, including areas that have narrowed or become blocked.
- Magnetic resonance angiography (MRA): Similar to a CTA, magnetic resonance angiography highlights blood vessel blockages.
- Pure volume recording (PVR): This test measures the variation in the volume of the lower limbs during the cardiac cycle. Reductions in the pulsatility may mean there are blockages. Doctors often combine this test with a Doppler ultrasound examination of the leg arteries.
- Ultrasound: An ultrasound uses sound waves to allow healthcare professionals to see blood circulation through the arteries and veins.
Effective PVD treatment aims to slow or stop disease progression, manage pain and other symptoms, and reduce the risk of serious complications.
PVD treatment plans usually involve lifestyle changes. Some people may also require medication, and severe cases may require surgical treatment.
Lifestyle changes
Lifestyle changes include:
- engaging in regular exercise, including walking
- eating a balanced, nutritious diet
- losing weight if a doctor has recommended it
- quitting smoking
Medication
Medications to treat PVD include:
- cilostazol: reduces claudication symptoms, such as muscle pain or fatigue
- clopidogrel or aspirin: prevents platelets from clumping together on top of plaque buildup
- pentoxifylline: also treats claudication, but is an older drug occasionally prescribed for individuals who cannot take cilostazol
Co-occurring conditions may also require medications to keep symptoms under control. For example, some people may need:
- statins (such as atorvastatin and simvastatin) to reduce high cholesterol
- angiotensin-converting enzyme (ACE) inhibitors for hypertension
- metformin or other diabetes medications to manage blood sugar
Surgery
People with severe PVD might require surgery to widen arteries or bypass blockages. Surgical options include:
- Angioplasty: This procedure involves inserting a catheter fitted with a balloon into the damaged artery and then inflating the balloon to widen the artery. Sometimes, the doctor will place a small tube (stent) in the artery to keep it open.
- Vascular bypass surgery: Also known as a vascular graft, this procedure involves reconnecting blood vessels to bypass a narrow or blocked part of a vessel. It allows blood to flow more easily from one area to another.
If PVD is left undiagnosed and untreated, it can cause severe or life threatening complications, such as:
- gangrene (tissue death), which can require amputation of the affected limb
- severe pain that restricts mobility
- slow-healing wounds
- potentially fatal infections of the bones and blood
A person can reduce their risk of developing PVD by engaging in behaviors that help lower their chance of developing many other chronic diseases. Some of these behaviors include:
- quitting smoking, or not starting
- getting daily physical activity, such as walking, biking, doing yoga, or going to a gym
- eating a balanced, nutritious diet that focuses on whole foods
- maintaining a moderate body weight
- managing blood sugar, cholesterol, and blood pressure levels
When diagnosed early, PVD is often easily treated with lifestyle modifications and medications.
A doctor can monitor a person’s improvement by measuring the distance they can walk without claudication. If treatments are effective, people should be able to gradually walk longer distances without pain.
Early intervention may prevent the condition from progressing and can help a person avoid complications. Anyone experiencing any of the symptoms of PVD should see a doctor.
The sudden development of pale, cold, and aching limbs with loss of pulses is a medical emergency and requires immediate treatment.
